Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Bowel Resection
Surgery Overview
Resection is another name for any surgery that removes tissue or part of an organ. Bowel resection removes a diseased or damaged part of the small intestine, large intestine (colon), or rectum. Bowel resection can be done for many diseases that affect the colon, such as colorectal cancer, diverticulitis, or Crohn's disease.
The goal of bowel resection is to take out the part of the bowel where the problem is. If the doctor is removing cancer from the colon, nearby lymph nodes are taken out and tested for cancer. Then healthy ends of the colon or rectum are sewn back together. Bowel resection is done either by opening the abdomen (open resection) or by laparoscopy.
Laparoscopy for bowel resection usually involves 3 to 6 very small incisions instead of one large one. Recovery time is often faster.
You and your doctor will think about several things in deciding whether you should have open resection or a laparoscopy. These include:
- The location and extent of the disease.
- Your general health.
- Whether you have scar tissue in the area from previous surgery.
- Your doctor's expertise and experience.
Sometimes a laparoscopic surgery has to be changed to an open resection during the surgery.
How It Is Done
Colon problems
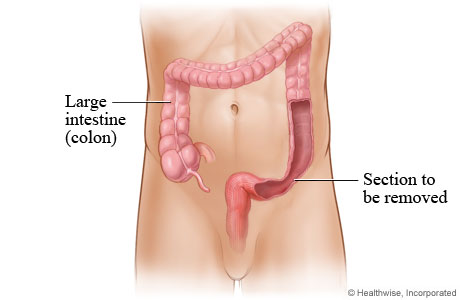
A partial colectomy is surgery to remove part of the large intestine (colon). This surgery is often needed for health problems such as diverticulitis, colon cancer, Crohn's disease, or colitis. These diseases can lead to problems with the colon, such as blockage, inflammation, lack of blood supply, or perforation.
A partial colectomy is also called a bowel resection.
Colon section removed
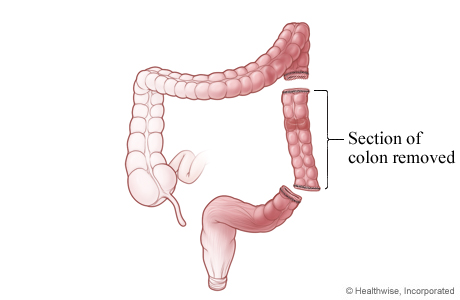
First, the surgeon removes part of your colon.
Colon ends reattached
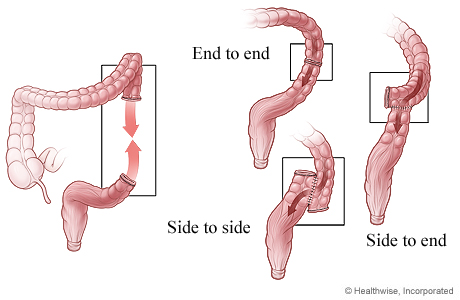
In many cases, the surgeon can reattach the ends of the colon in the same surgery. The ends can be reattached end to end, side to side, or side to end.
But sometimes the ends can't be reattached until the colon has had some time to heal. In this case, the surgeon will need to create a stoma.
Stoma created
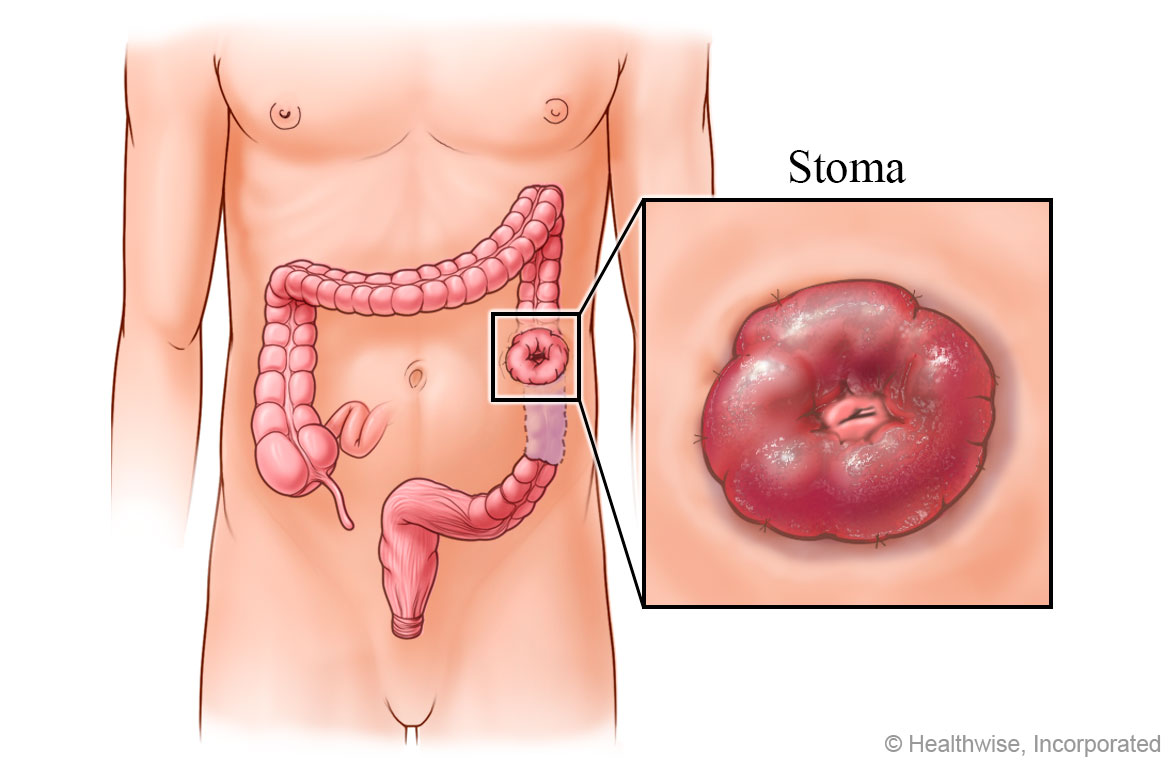
To create a stoma, the surgeon makes an opening in your belly and connects part of the intestine to that opening in the skin. This opening is the stoma.
After you have this surgery, which is called a colostomy, waste will leave your body through the stoma instead of through the anus.
This completes the first surgery. You then have to give your colon time to heal.
Colostomy bag in place
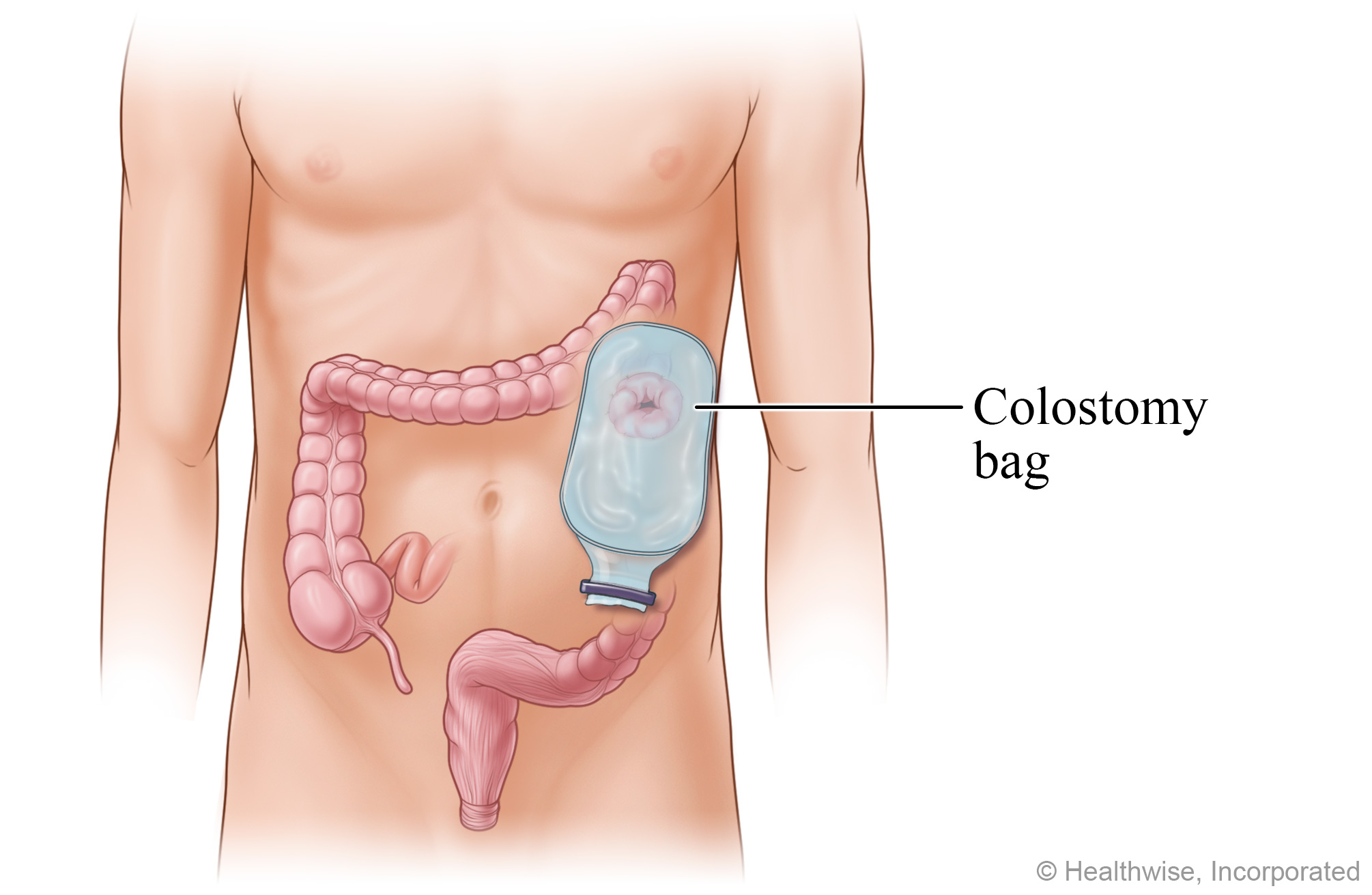
There is no muscle around the stoma, so you won't be able to control when waste or gas passes out of your body. To collect the waste, an odor-proof plastic colostomy bag (also called an ostomy pouch) is placed on the stoma. The bag is held to your skin with an adhesive or tape. Body waste passes from the colon through the stoma into the colostomy bag.
After your colon has healed, you may be able to have another surgery to close the stoma and reattach the ends of your colon. After the ends of your colon are reattached, you will no longer need a colostomy bag. Waste will again leave your body through the anus.
What To Expect
Bowel resection requires general anesthesia. You may stay in the hospital for 4 to 7 days or as long as 2 weeks after surgery.
Sometimes the two parts of the colon or rectum can't be reattached, so the surgeon performs a colostomy. This creates an opening, called a stoma, on the outside of the body for the stool, or feces, to pass through into a colostomy bag. Usually the colostomy is temporary, until the colon or rectum heals. If the lower part of the rectum has been removed, the colostomy is permanent.
When the two-stage surgery is done, the time between surgeries is usually 6 to 12 weeks.
The recovery time after each surgery is usually 6 to 8 weeks.
Why It Is Done
Bowel resection may be done to remove cancer or when the bowel cannot function normally because of damage or disease. You may need a bowel resection if you have:
- A bowel obstruction.
- Colon cancer.
- Crohn's disease.
- Diverticulitis.
How Well It Works
Most people who have surgery for invasive cancer do not have the tumor return. The likelihood of success depends on many factors, such as the stage of the cancer.footnote 1
A small number of people who have surgery for diverticulitis develop diverticulitis again within 5 years. But another surgery is usually not needed.
Surgery is not a cure for Crohn's disease. When surgery for Crohn's is needed, as little of the intestine as possible is removed to keep the intestines working normally. The disease tends to return to other areas of the intestines after surgery. About one-quarter of Crohn's disease patients who have a first surgery also have a second. And many of these second ones are within 5 years of the first surgery.footnote 2 In children, surgery may improve well-being and quality of life and restore normal growth and sexual development.
If a colostomy is needed during the bowel resection, usually it is temporary, until the colon or rectum heals. If the lower part of the rectum has been removed, the colostomy is permanent.
Risks
All surgeries have some risks of infection, severe bleeding, or complications from general anesthesia.
Possible problems after a bowel resection include:
- Scar tissue (adhesions).
- A leak between the joined sections of the colon.
- Injury to the bladder, ureters, or blood vessels.
References
Citations
- Vogel JD, et al. (2022). The American Society of Colon and Rectal Surgeons clinical practice guidelines for the management of colon cancer. Diseases of the Colon and Rectum, 65(2): 148–177. DOI: 10.1097/DCR.0000000000002323. Accessed December 7, 2023.
- Frolkis AD, et al. (2014). Cumulative incidence of second intestinal resection in Crohn's disease: A systematic review and meta-analysis of population-based studies. American Journal of Gastroenterology, 109(11): 1739–1748. DOI: 10.1038/ajg.2014.297. Accessed December 7, 2023.
Credits
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.






