Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Aortic Valve Replacement Surgery
Surgery Overview
Aortic valve replacement gives you a new aortic heart valve. The new valve may be mechanical or made of animal tissue. You and your doctor can decide before surgery which type of valve is best for you.
The aortic valve opens and closes to keep blood flowing in the proper direction through your heart. When the aortic valve does not close properly, it's called aortic valve regurgitation. If the valve is very tight and narrow, it's called aortic valve stenosis. In both of these cases, blood does not flow through the heart the right way.
You will be asleep during the surgery. In an open-chest surgery, your doctor will make a cut in the skin over your breastbone (sternum). This cut is called an incision. Then the doctor will cut through your sternum to reach your heart. In a less invasive surgery, your doctor will make a cut between your ribs. Your sternum is not cut.
The doctor will connect you to a heart-lung bypass machine. It adds oxygen to your blood and moves the blood through your body. This machine will allow the doctor to stop your heartbeat and replace the valve.
After the doctor has replaced your aortic valve, the doctor will restart your heartbeat. Then the doctor may use wire to put your sternum back together. Your incision will be closed with stitches or staples. The wire will stay in your chest. The incision will leave a scar that may fade with time.
You may stay in the hospital for a few days after surgery.
How It Is Done
In open-heart surgery, the surgeon makes an incision in the middle of the chest
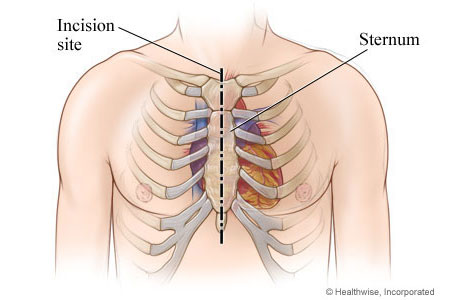
Aortic valve replacement surgery may be done as an open-heart surgery or as a less invasive surgery. In open-heart surgery, the surgeon makes an incision in the middle of the chest and cuts through the breastbone (sternum). In less invasive surgery, the surgeon makes smaller incisions and does not open the chest.
In less invasive surgery, the surgeon may make an incision between the ribs
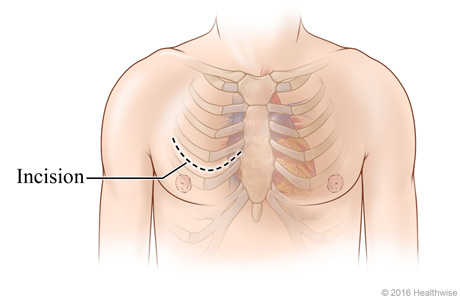
In a less invasive surgery, the surgeon may make an incision between the ribs. The surgeon uses this incision to work on the heart. The surgeon does not cut the sternum.
The chest is opened to expose the heart
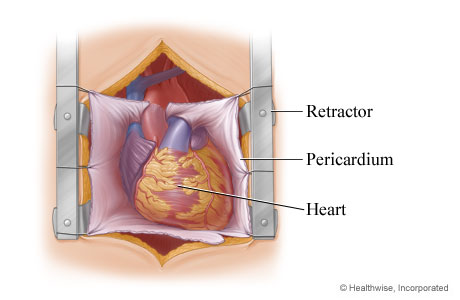
In an open-heart surgery, the surgeon opens the chest with a retractor to expose the heart. The surgeon opens the lining that protects the heart (pericardium).
The damaged aortic valve is removed
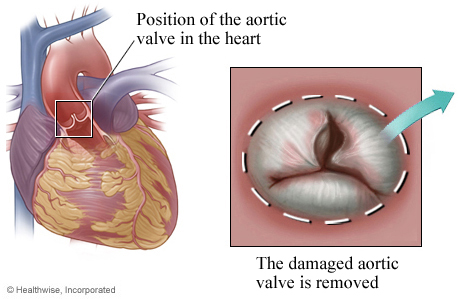
Next, the surgeon removes the damaged aortic valve.
The replacement valve is sewn in place
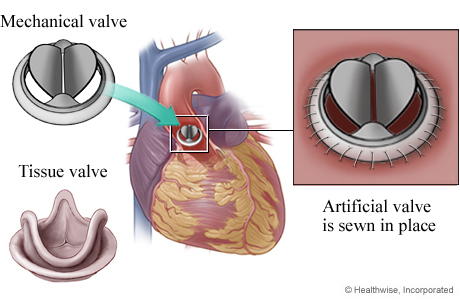
Finally, the surgeon inserts the replacement valve into the aorta. The replacement valve may be either mechanical or made of animal tissue. The surgeon sews the valve to the annulus, which is a ring of tissue that connects to the leaflets of the aortic valve.
What To Expect
You will recover in the hospital until you are healthy enough to go home. Depending on your overall health, you may go home a few days after surgery.
Surgery will likely involve a long recovery over several weeks. You will probably need to take 4 to 12 weeks off from work. It depends on the type of work you do and how you feel. In some cases, full recovery may take several months.
Your doctor may suggest that you attend a cardiac rehab program. In cardiac rehab, a team of health professionals provides education and support to help you recover and prevent problems with your heart. Ask your doctor if rehab is right for you.
Learn more
Why It Is Done
Aortic valve regurgitation
If your chronic regurgitation is getting worse and you have symptoms, you may choose to have surgery. You might have surgery before you get symptoms, especially if your regurgitation is getting worse. If you have acute regurgitation, surgery will likely be done right away.footnote 1
Aortic valve stenosis
Valve replacement is recommended based on many things including how severe the stenosis is, whether you have symptoms, and how well your heart is pumping blood. It is typically recommended when a person has severe stenosis.footnote 1
Learn more
How Well It Works
Aortic valve regurgitation
Valve replacement surgery helps relieve symptoms and prevent heart failure. And it helps people live longer.
Aortic valve stenosis
Valve replacement surgery is an effective treatment for people who have severe aortic valve stenosis. Surgery can relieve symptoms, improve your quality of life, and help you live longer.
Risks
The risks of aortic valve replacement surgery vary depending on your age and general health before surgery. Younger, healthy people have a lower risk of problems, while older people with other health problems have a higher risk.
In general, the risks include:
- Effects from the surgery itself. These include:
- Bleeding.
- Infection.
- Risks from anesthesia.
- Atrial fibrillation.
- Heart attack.
- Stroke.
- Heart attack and stroke.
- Death from the surgery. This risk can be higher or lower depending on many things such as age, heart health, and other medical problems.
- Blood clots caused by the new valve. Replacement with a mechanical valve requires lifelong treatment with anticoagulant medicine to prevent dangerous blood clots.
- Infection around the replacement valve.
- Failure of the new valve. There is a small chance that the valve will not work. Your doctor will need to check from time to time to make sure that your valve is working.
- The need for another valve replacement surgery. Replacement valves last only for a limited time. Having valve surgery again will depend on what type of valve you have and how long you live after your first surgery.
Credits
Current as of: October 2, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 2, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.




